In modern obstetrics, cesarean sections, once vital life-saving procedures, have become overutilized, often without medical necessity. In Pakistan, this alarming trend, fueled by financial motives, convenience, and inadequate healthcare understanding, not only jeopardizes maternal and infant health but violates fundamental human rights.
A C-section is a major surgical procedure where a baby is delivered through an incision in the mother’s abdomen. While it can be essential for complications during labor, its growing frequency suggests that many are being performed without sound medical reasons. Alarmingly, studies indicate that over half of cesarean deliveries in Pakistan are unnecessary. Private hospitals, driven by financial motives, often prefer C-sections because they are quicker, more profitable, and yield higher revenue than a natural delivery. The procedure typically takes only 8 to 10 minutes, compared to the prolonged hours of labor involved in vaginal births, which can extend over 12-14 hours. This convenience, unfortunately, comes at a tremendous cost to the health of both the mother and the child.
The ethical concerns surrounding the overuse of C-sections are particularly troubling when considering first-time pregnancies. It is widely accepted in medical practice that the first labor, while often longer and more painful, is critical for doctors and midwives to assess the progress of the birth. In Pakistan’s public healthcare, the absence of pain relief, such as epidurals, forces many women into unnecessary C-sections to escape the agony, further escalating this troubling trend.
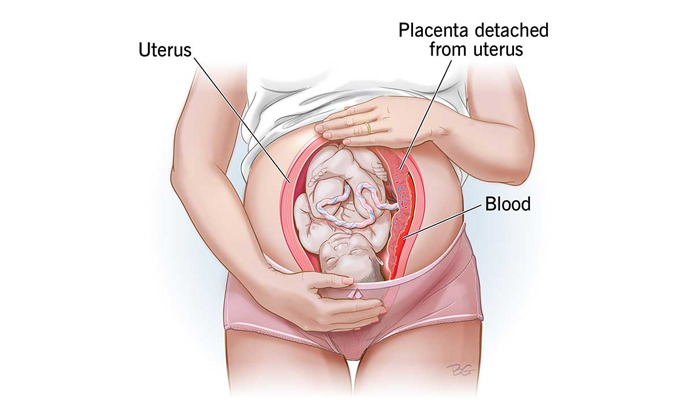
At the heart of this issue lies a fundamental breach of the medical principle of "do no harm." C-sections, though life-saving when necessary, carry significant risks, including infections, excessive bleeding, scarring, complications in future pregnancies, and even maternal death. Moreover, bypassing a natural vaginal birth, which generally carries fewer risks, deprives the mother of a safer and less invasive option. This disregard for the health and dignity of women is not only unethical but, in many ways, a violation of their human rights.
An even more alarming aspect of this crisis is the emotional manipulation of expectant mothers. Doctors often exploit the fears and anxieties that accompany childbirth, particularly for first-time parents, by presenting exaggerated, unlikely scenarios as justification for a C-section. Conditions such as an umbilical cord wrapped around the baby’s neck, a drop in the baby’s heart rate, or low amniotic fluid are sometimes used as reasons for immediate surgery. While these complications can sometimes occur, they are often manageable during vaginal delivery without the need for a C-section. Yet, doctors may use these scenarios as emotional blackmail, convincing mothers that a C-section is the only way to "save" their child, thereby instilling fear and preventing them from considering other, less invasive options.
The financial incentives behind this trend cannot be overlooked. C-sections are more profitable for hospitals than vaginal deliveries, this procedure can generate substantial revenue. The quick turnaround time of a C-section, which takes only minutes compared to the long hours of labor involved in vaginal births, makes it an attractive choice for doctors seeking to maximize their time. This economic pressure often results in unnecessary surgeries being performed, with the financial gain of the healthcare provider outweighing the potential risks to the mother and baby.Unnecessary C-sections not only endanger women with infections and long-term complications but also jeopardize infants, leading to respiratory issues and developmental delays. As C-section rates soar, Pakistan’s overtaxed healthcare system buckles under the weight of this growing crisis, with lasting repercussions for both health and policy.
Pakistan, already grappling with one of the highest maternal mortality rates globally, has witnessed its cesarean rates more than double in the past two decades. According to the World Health Organization (WHO), the ideal cesarean section rate should range from 10-15%. When rates exceed this range, there is no substantial improvement in maternal mortality. Instead, the health risks for both mother and child increase.
We call upon all stakeholders healthcare providers, policymakers, and families to recognize the importance of informed consent and the ethical obligation to ensure that C-sections are performed only when truly necessary. The health of mothers and children should always come first. Let us work together to preserve the dignity, rights, and well-being of every woman and child, ensuring that medical interventions are always in their best interests.
This Opinion has been written by Dr Sidra Ahmed.